Intended Learning Outcomes
Section 1 (Introduction and review of respiratory physiology)
Introduction
- course introduction
Introduction to cardiopulmonary physiotherapy
- appreciate the various services provided by a cardiopulmonary physiotherapist
- identify clients that require cardiopulmonary physiotherapy
- understand the role of a cardiopulmonary physiotherapist in acute care, outpatient and community settings
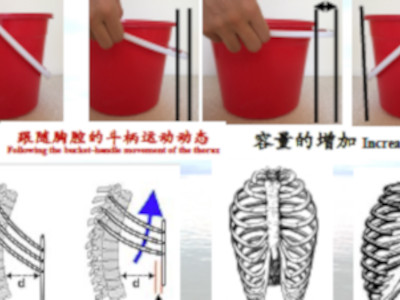
Review of respiratory physiology: mechanics of breathing
- explain the physiology underpinning respiratory techniques commonly employed by a respiratory physiotherapist, such as cough, huff and breathing exercise
- apply the concepts of equal pressure point, airway and elastic resistance, pulmonary compliance, work of breathing, and the relationship between pleural pressure, alveolar expansion and ventilation, to assist with clinical decisions associated with positioning of patients and the selection of appropriate interventions that address issues relevant to a patient’s respiratory mechanics
Review of respiratory physiology: ventilation and perfusion relationship
- explain the regional variation of ventilation and perfusion within the lungs
- identify factors that influence intrapulmonary shunting of blood
- provide reasoning for selection of an appropriate position to maximise lung volume and/or ventilation
- determine an appropriate strategy to maximise oxygenation through positioning
Oxygen therapy
- apply various oxygen delivery systems to a patient
- facilitate appropriate oxygen therapy to a patient
- advise patients on the use of supplementary oxygen as appropriate
- understand the risks of supplementary oxygen
Humidification and inhalation therapy
- make clinical decision as to whether inhalation therapy (humidification or nebulisation) is indicated for a patient
- apply appropriate means to improve humidification of the airway
- teach the patient proper use of an nebuliser
- instruct patients the appropriate use of various meter dosed inhalers
Section 2 (Physiotherapy assessment and cardiopulmonary physiotherapy intervention)
Understanding spirometry
- conduct an accurate spirometry test
- interpret the numerical and graphical spirometry data
- recognise the various spirometry patterns associated with restrictive and obstructive pulmonary disease
- appreciate the American Thoracic Society recommendations for presenting spirometry test data
- appropriately use spirometry data as an outcome measure to evaluate a physiotherapy intervention
Assessment of respiratory function
- conduct a patient interview and ask appropriate questioning relating to a patient’s respiratory condition
- perform essential physical examination procedures in a patient with respiratory disease
- identify a patient’s problems from assessment findings in order of importance from the clinical evidence
- relate assessment findings to the pathophysiological presentation
- monitor appropriate measurable outcomes as indicators of progression of the patient’s respiratory condition
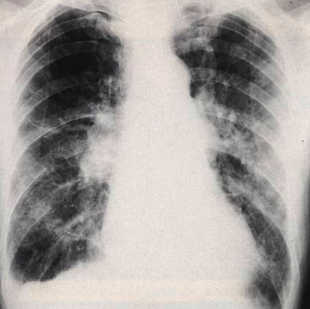
An overview of objective data which reflect the level of respiratory function
- identify abnormal oxygenation and ventilation in a patient by interpretating a blood gases analysis profile and pulse oximetry
- interpret spirometric analysis of lung volume and airflow
- interpret normal and abnormal features of a chest radiograph
- measure an exhaled carbon monoxide level
- appreciate the role of thoracic ultrasound in monitoring breathing pattern and diaphragm thickness
Airway Clearance Techniques
- describe the concept of airway clearance
- select an airway clearance technique (ACT), underpinned by current best evidence, that is appropriate to the patient’s pathophysiological condition
- apply the appropriate airway clearance techniques covered in the lecture
- evaluate the effectiveness of an ACT with appropriate outcome measures
- make clinical decision regarding the needs of adjunctive therapy devices to assist airway clearance
Techniques to improve lung volume and ventilation
- identify indications for the need to employ techniques to improve a patient’s ventilation or lung volume
- perform techniques commonly used by physiotherapists to promote pulmonary ventilation
- based on the patient’s pathophysiological condition, make clinical decision on selection of the appropriate technique for improvement of lung volume or ventilation
Role of Physiotherapy in Pre and post-surgical care
- identify risk factors that may contribute to post-surgical pulmonary complications
- appropriately provide pre- and post-surgical physiotherapy intervention
- deliver a pre-operative patient assessment and provide appropriate pre-operative advice and intervention for the patient
- conduct an appropriate post-operative assessment
- perform appropriate intervention following assessment outcome of the patient
- consider discharge criteria for a patient
- formulate a comprehensive discharge plan for the patient prior to returning home




Section 3 (Management of COPD, pulmonary rehabilitation and paediatric care)
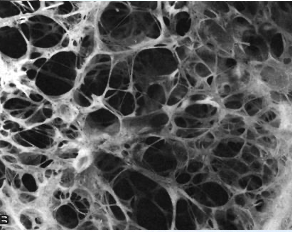
Management of patients with COPD
- describe the pathophysiology, diagnosis, signs and symptoms of Chronic Obstructive Pulmonary Disease (COPD)
- explain mainstream medical management
- conduct an appropriate physiotherapy assessment using the ICF framework
- provide intervention and education for patients with COPD
- select appropriate outcome measures to determine effectiveness of the management program
- be aware of the risks of supplementary oxygen administration in patients with COPD
- identify global management guidelines for COPD
Management of patients with lung cancer
- describe the causes, risk factors and types of lung cancer
- aware of diagnostic methods of lung cancer
- outline the different stages of lung cancer
- understand the contemporary medical management of patients with lung cancer
- comprehend the role of physiotherapy in exercise management of patients with lung cancer
- appreciate the role of physiotherapy in pre and post-operative management of patients with lung cancer
- recognise the role of a physiotherapist in the prevention of lung cancer
Pulmonary rehabilitation and exercise prescription
- identify and prioritise each patient’s needs for pulmonary rehabilitation
- work with the patient to identify SMART goals during the various stages of pulmonary rehabilitation
- prescribe an appropriate individual exercise program based on patient assessment
- work collaboratively with other members of the pulmonary rehabilitation team
Physiotherapy management of paediatric patients
- identify the anatomical differences in the adult and neonatal respiratory system
- consider an appropriate position to maximise lung volume or ventilation in a neonate
- recognise the role of physiotherapy at different stages of common paediatric respiratory conditions
- identify the indications for physiotherapy in children with spinal muscular atrophy (SMA)
- assess the need for and provide, appropriate pre and post operative interventions, in children undergoing orthopaedic and cardiac surgery
Prescribing breathing devices in respiratory care
- understand the working mechanisms of different breathing devices
- recognise indications for use of a breathing device in the appropriate patient
- provide clear instructions to patients on the use of a breathing device
- provide prescription of an appropriate program to a patient which may benefit from the use of a breathing device
Section 4 (Cardiac rehabilitation)
Management of Cardiovascular disease
- define different type of cardiovascular diseases
- describe the relevant pathophysiology and risk factors of various cardiovascular diseases and heart failure
- explain various methods of diagnosis coronary artery disease
- aware of the clinical pathway for management of acute coronary syndrome and heart failur
- assess and monitor variable risk factors of cardiovascular disease
- understand the role of physiotherapy in management of clients with or at risk of cardiovascular disease
Cardiac Surgery - implications for physiotherapists
- understand the current surgical management of patients with cardiac and cardiovascular disease: including coronary artery bypass grafting, valvular repair and replacement, implantable devices, aortic aneurysm, aortic dissection and pectoral flap advancement
- appreciate the role of physiotherapy in common cardiac surgical procedures in patients with concurrent cardiovascular disease
- provide appropriate advice to patients after sternotomy
- be aware of safety precautions associated with exercise prescription for patients with implantable devices
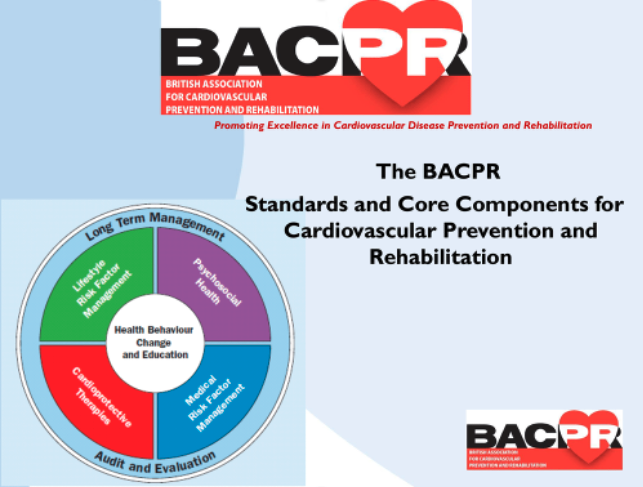
Overview of cardiac rehabilitation
- explain to clients and relevant stake holders the evolution of cardiac rehabilitation
- explain the concepts of cardiac rehabilitation
- select appropriate candidates for a cardiac rehabilitation program
- refer clients to an appropriate cardiac rehabilitation service
- participate in the planning and/or organisation of a cardiac rehabilitation program
- apply appropriate indicators to evaluate the quality of a cardiac rehabilitation program
- collaborate with other professions in the various domains of a cardiac rehabilitation program
Role of physiotherapy in phase I cardiac rehabilitation
- explain the role of physiotherapy in management for patients with cardiac conditions that require hospitalisation
- retrieve relevant information from the patient’s hospital notes
- assess the cardiac and haemodynamic status of the patient
- identify and prioritise the patient’s problems
- formulate a safe and appropriate intervention plan for a patient after acute cardiac event including myocardial infarction, acute coronary syndrome and cardiac surgery
- formulate appropriate physiotherapy discharge criteria for a patient admitted for cardiac management
Phase II cardiac rehabilitation - assessment, goal setting and exercise prescription
- assess the individual needs of participants recruited to a cardiac rehabilitation program
- develop a comprehensive plan of care for participants in a cardiac rehabilitation program
- work collaboratively with other members of the cardiac rehabilitation team in assessment and goal-setting for participants undertaking a Phase II cardiac rehabilitation program
- apply the principle of exercise prescription to participants in a cardiac rehabilitation program
- modify the exercise protocol based on the patient’s responses to exercise training
- document the mode of exercise and patient response following each exercise session
- prescribe an individualised home exercise program for a patient based on the patient’s response to supervised exercise
- evaluate the effectiveness of an exercise program





Section 5 (Physiotherapy in ICU care)
Introduction to intensive care and monitoring in an ICU
- understand the organisation and management of an ICU
- describe the general management of the critically ill in the ICU
- explain the need for early mobilisation in ICU patients
- describe the commonly used outcome measures that reflect the oxygenation status of an ICU patient
- describe and interpret capnogram data
- describe and interpret the data which provide the haemodynamic profile of a patient
- interpret the data elicited by various neurological assessment tools
- explain and perform a Physical Function ICU Test and ICU mobility test
- work together with the ICU team in proning an intubated patient
- work collaboratively with other members in the ICU team
Principle of mechanical ventilation
- define the types of respiratory failure
- explain the indications for mechanical ventilation
- describe common modes of mechanical ventilation
- understand the concept of lung recruitment
- appreciate the role of physiotherapist during weaning from mechanical ventilation
Manual hyperinflation (MHI), ventilator hyperinflation (VHI) and non-invasive ventilation (NIV)
- describe the process of manual hyperinflation
- select appropriate patients who will benefit from manual hyperinflation
- describe the process of ventilator hyperinflation
- understand various protocols of VHI reported in the literature
- describe and apply appropriate selection criteria for patients to undergo ventilator hyperinflation
- explain the clinical use of non-invasive ventilation
Role of physiotherapy in ICU care
- describe the role of a physiotherapist in ICU
- provide an appropriate assessment for physiotherapy procedure in ICU
- recognise factors that inhibit patient mobilisation in ICU
- apply appropriate outcome measures to determine effectiveness of physiotherapy care delivered in an ICU environment
Role of physiotherapy in management of acute and post- COVID-19
- describe the pathophysiology of COVID-19 and clinical presentation of the disease
- aware of the global current variants of concerns
- understand the role of physiotherapy in acute management of patients with COVID-19
- recognise the risk of silence hypoxia in people with COVID-19
- appreciate the special considerations necessary for delivery of pulmonary rehabilitation of patients with post-COVID-19
- understand the role of physiotherapy in public health promotion and prevention of COVID-19 infection
Physiotherapy documentation
- understand the need to document every physiotherapy assessment, intervention and outcome
- document a patient’s consent to physiotherapy assessment and interventio
- document a patient’s past medical history, social history, subjective, and objective assessment findings
- document an intervention plan for the patient